Flu Fighter: Dr. James Stevens, Ph.D.
CDC’s influenza laboratories play a leading role in the ongoing global task of looking for new flu viruses, assessing the risk they pose to people, and supporting efforts to proactively prepare for the emergence of flu viruses considered to have pandemic potential. This includes everything from conducting surveillance on novel influenza viruses, to developing the viruses that are used to mass-produce flu vaccines, which are called “candidate vaccine viruses” or “CVVs”. As Associate Director for Laboratory Sciences in CDC’s Influenza Division, Dr. James Stevens oversees and coordinates CDC’s influenza laboratory operations. He says the 1918 flu pandemic “is the deadliest we’ve seen in modern times. We have to remember it because it is the worst-case scenario situation, and we don’t want it to happen again.”
As Associate Director for Laboratory Sciences in CDC’s Influenza Division, Dr. James Stevens says “Every novel flu virus that comes in our doors is treated like a pandemic-potential virus.”
Why the 1918 Pandemic Still Matters
A novel flu virus is one that does not routinely infect and spread in people. While seasonal flu viruses place a large burden on the health of Americans annually, novel flu viruses with pandemic potential can wreak devastation if they adapt to easily infect and spread between people. The 1918 pandemic is the most severe example of the damage a flu pandemic can cause. Since that time, Stevens says, “we have a lot more knowledge than we did 100 hundred years ago to be able to respond more quickly. Back then, we really didn’t know this disease was caused by a virus. We could only identify it based on symptoms. We now know not only that influenza illness is caused by a virus, but we have a global network to detect flu viruses, extensive research capacity to study them, and in terms of prevention and treatment, we have flu vaccines, we have laboratory testing, point of care diagnostics, and antiviral drugs for treatment.”
Being a Flu Fighter
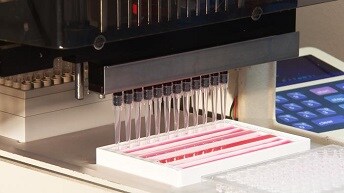
CDC’s global influenza virus surveillance program tracks human infections with novel flu viruses in addition to analyzing thousands of seasonal flu viruses each year. More than 6,000 flu viruses undergo full genetic sequencing as a first step after they arrive at CDC. Most of these are seasonal flu viruses, but dozens are novel flu viruses that have infected people, sometimes for the first time. “Influenza viruses constantly change. They are some of the fastest mutating viruses we know, and so it’s a constant struggle to keep on top of them. That’s why genetic sequencing of flu viruses—both seasonal and novel—is so important. Genetic sequencing can give us information about each virus based on decades of other laboratory work. For example, we have identified markers that have previously been associated with severe illness, or antiviral resistance, and if we see those markers in the genetic sequence of a newly detected novel flu virus, that gives us a heads up that this virus is important to look at further.”
Other laboratory research that has been ongoing for years takes a deeper dive into how fit the virus is (how well it spreads), what kind of disease it causes in animal models, whether or not the virus is susceptible to existing vaccines or antiviral drugs, and what level of immunity the general population might have against the virus. All of this research helps CDC assess the risk that a particular virus will evolve to cause a pandemic. For novel flu viruses with concerning pandemic potential, CDC labs then develop a candidate vaccine virus (CVV) that can be used by manufacturers to mass-produce flu vaccine.
Planning and Preparation are Critical; Challenges Remain
“The technology used to make most flu vaccines is more than 50 years old, but in the past 10 years there have been exciting innovations in how we can make a CVV,” Stevens says. “For decades, we were dependent on an original clinical specimen with live virus that we could then grow, manipulate and develop into a CVV. Today, we don’t need the actual virus. If we have the genetic sequence information, we can actually build the same virus in our labs and use it to make a CVV.” When a new sub-group of Asian A(H7N9) viruses emerged in China in 2017, Chinese public health officials posted the genetic sequence of the virus and CDC was able to make a virus based on that genetic sequence. That CVV, made using “reverse genetics” was used to make an A(H7N9) vaccine being tested in a clinical trial right now. Dr. Stevens also points out there’s a lot of work going on to develop universal flu vaccines. “These are vaccines which target more conserved regions of the virus, and will actually introduce a greater longevity in terms of the vaccine and its effectiveness. It will have a broader response as well.” Vaccines are the first and best line of defense against both seasonal flu and a flu pandemic. “We need to continue to improve current vaccines so that we can blunt the impact of the next pandemic,” Stevens says. While there is a lot of work still to be done, Dr. Stevens is confident. “We [CDC] have an extremely capable Division and we are committed in our fight against flu, both seasonal and pandemic.”