Influenza Vaccination Coverage Among Health Care Personnel — United States, 2019–20 Influenza Season
The Advisory Committee on Immunization Practices (ACIP) recommends that all health care personnel (HCP) receive an annual influenza vaccination to reduce influenza-related morbidity and mortality among HCP and their patients as well as to reduce absenteeism among HCP (1-4). CDC conducted an opt-in Internet panel survey of 2,401 U.S. HCP to estimate influenza vaccination coverage during the 2019–20 influenza season. Overall, 80.6% of HCP reported receiving influenza vaccination during the 2019–20 season, similar to reported coverage in the previous season. Coverage was higher among HCP who were required by their employer to be vaccinated (94.4%) than among those whose employer did not require vaccination (69.6%). By setting, vaccination coverage was highest among HCP in ambulatory care and hospital settings with vaccination requirements (96.1% and 95.7%, respectively), and lowest in ambulatory and long-term care settings without vaccination requirements, promotion, or on-site offer (47.7% and 49.9%, respectively). Implementing workplace strategies to improve vaccination coverage among HCP, particularly in long-term care settings, including active promotion of on-site vaccinations can help ensure HCP and patients are protected against influenza (5). Reducing the overall burden of respiratory illnesses in the upcoming season by maximizing HCP influenza vaccination uptake can help protect vulnerable populations including long-term care facility residents and conserve healthcare resources for treatment of COVID-19.
An Internet panel survey of HCP was conducted during March 31–April 30, 2020, to provide estimates of influenza vaccination coverage among HCP during the 2019–20 influenza season. Similar surveys have been conducted since the 2010–11 influenza season, and survey methodology has been described previously (6). Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network,* and general population Internet panels operated by Dynata (formerly known as Survey Sampling International (SSI)).† Responses were weighted to the distribution of the U.S. population of HCP by occupation, age, sex, race/ethnicity, work setting, and Census region.‡ Because the study sample was based on HCP from opt-in Internet panels rather than probability samples, statistical tests were not conducted.§ A change of at least 5 percentage points between estimates has consistently been used with this survey to denote an increase or decrease; estimates with smaller differences were considered similar (6,7).
Among the 2,544 persons who started the survey from either source (Medscape or Dynata) and met eligibility criteria based on responses to the screening questions (i.e., were not screened out due to employment status, work setting, occupation, sampling targets having been met, or incomplete response to the screening questions), 2,454 (96.5%) individuals completed the survey.|| Fifty-three respondents (2.2%) with completed surveys who reported working in “other health care settings” were excluded because examination of their survey responses indicated that they were either unlikely to have contact with patients or unlikely to have worked in one of the health care settings of interest for this analysis. The final analytic sample included 2,401 HCP.
Overall, 80.6% of HCP reported having received an influenza vaccination during the 2019–20 season, similar to the previous season, but an increase from 63.5% in the 2010-11 season (Figure). During the 2019-20 season, vaccination coverage increased 9.9 percentage points from the last season to 82.7% among those aged ≥65 years. Highest vaccination coverage was observed among Hispanic (82.7%) and non-Hispanic white HCP (82.6%); lowest coverage was observed among non-Hispanic black HCP (73.6%). Vaccination coverage was highest among physicians (98.0%), followed by nurses (92.0%) and pharmacists (90.6%). Lowest vaccination coverages were reported among assistants and aides (72.4%) and non-clinical HCP (76.7%) (Table 1). Among HCP who reported a health condition that increases the risk for severe illness and complications from influenza, 82.1% reported influenza vaccination, ranging from 61.9%-91.2% across employer vaccination policies (Table 2).
Overall, 44.2% of HCP reported vaccination was required at their workplace (Table 2). As in the previous season, HCP working in settings where vaccination was required reported higher vaccination coverage (94.4%) compared with settings where vaccination was not required, promoted, or offered on-site (52.3%). Among work-related characteristics, overall vaccination coverage was highest in hospital settings (93.2%) and lowest in long-term care settings (69.3%). Within work setting, vaccination coverage was highest among HCP in ambulatory care and hospital settings with vaccination requirements (96.1% and 95.7%, respectively), and lowest in ambulatory and long-term care settings without vaccination requirements, promotion, or on-site offer (47.7% and 49.9%, respectively). Employer vaccination requirements, onsite vaccination availability and other vaccination promotions resulted in higher vaccination coverage regardless of work setting, presence of any high-risk condition, and occupation type (Table 2).
Overall influenza vaccination coverage among HCP was 80.6% during the 2019–20 season, a 17 percentage point increase since the 2010–11 season, but similar to the previous season. Higher vaccination coverage was observed among Hispanic and non-Hispanic white HCP and those in work settings where employers required vaccination. Lower vaccination rates were observed among non-Hispanic black HCP, and those in long-term care settings and work settings without vaccination requirements, promotion, or on-site offer. Regardless of characteristics such as work setting, presence of a high-risk condition or occupation type, vaccination coverage was as much as 48 percentage points higher among HCP with employer vaccination requirements compared with HCP without vaccination requirements, promotion, or on-site offer.
Findings from this survey indicate that many HCP, such as assistants/aides, other clinical personnel and non-clinical personnel, are unvaccinated, highlighting the need for more intensive interventions to improve annual influenza vaccination among different racial groups, in work settings, and in settings without employer vaccination requirements. Beneficial resources include CDC’s long-term care web-based toolkit,¶ which provides access to resources, strategies and educational materials, and interventions recommended by the Community Preventive Services Task Force, including providing and actively promoting on-site vaccination at no cost (5). These resources can be used by health care employers to increase influenza vaccination coverage among HCP and reduce influenza-associated morbidity and mortality among patients. Furthermore, routine monitoring and reporting of vaccine coverage by race/ethnicity and other socio-demographic factors might also help reduce racial and ethnic vaccination differences (8).
Finally, with the COVID-19 pandemic, it is especially important to implement systems that support and encourage the overall vaccination of HCP, in particular those working at long-term care facilities. Previous findings have demonstrated that outbreaks of COVID-19 in these settings have a critical impact on the health of vulnerable older adults (9). Given the low vaccination coverage among HCP in long-term care facilities (69.3%) in the 2019-20 season, efforts will be needed to improve influenza vaccination uptake among these HCP to better protect residents and themselves. Many of the long-established public health actions to increase influenza vaccination coverage among HCP can be used not only for routine vaccinations but also for COVID-19 vaccine when it becomes available.
The findings in this report are subject to at least four limitations. First, the study used a nonprobability sample of volunteer members of Medscape and Dynata Internet panels, which might affect the generalizability of these findings to the U.S. HCP population even after responses were weighted to be representative of the U.S. population of HCP. Second, vaccination status was self-reported and may be subject to recall bias. Third, statistical tests were not conducted and statistically significant differences between groups were not measured due to using a nonprobability sample. Finally, coverage findings from Internet survey panels have differed from population-based estimates from the National Health Interview Survey in past influenza seasons, although trends in coverage were similar across seasons (10).
FIGURE. Percentage of health care personnel who received influenza vaccination, by work setting* — Internet panel surveys,† United States, 2010–11 through 2018–19 influenza seasons
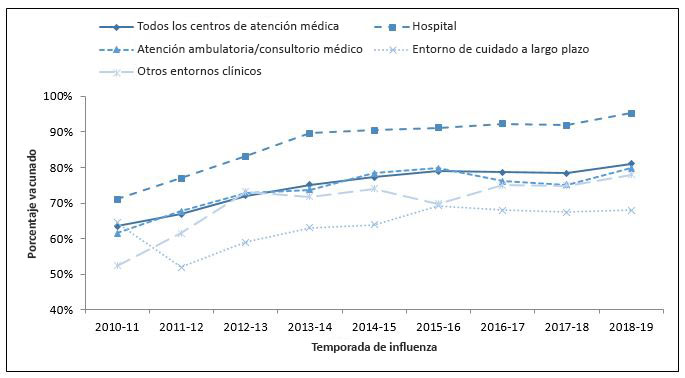
* Persons who worked in a place where clinical care or related services were provided to patients, or whose work involved face-to-face contact with patients or who were ever in the same room as patients.
† Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata.
Table 1: Percentage of health care personnel* who received influenza vaccination by demographic and work-related characteristics, Internet panel surveys,† United States, April 2020
|
2018-19 |
2019-20 |
Percentage-point difference (2018–19 to 2019–20) |
|||
|---|---|---|---|---|---|
|
No. (weighted %‡) |
Weighted % vaccinated |
No. (weighted %‡) |
Weighted % vaccinated |
||
|
Total |
2,386 (100.0) |
81.1 |
2,401 |
80.6 |
-0.5 |
| Age Group | |||||
| 18-49 years | 1,586 (65.4) | 81.5 | 1,615 (67.9) | 79.1 | -2.4 |
| 50-64 years | 669 (28.8) | 81.8 | 640 (25.8) | 84.0 | 2.2 |
| ≥65 years | 131 (5.8) | 72.8 | 146 (6.3) | 82.7 | 9.9 |
| Race/ethnicity§ | |||||
| White, non-Hispanic | 1542 (63.2) | 80.8 | 1494 (61.1) | 82.6 | 1.8 |
| Black, non-Hispanic | 294 (15.0) | 77.2 | 302 (14.6) | 73.6 | -3.6 |
| Hispanic | 308 (13.9) | 85.5 | 334 (14.8) | 82.7 | -2.8 |
| Other, non-Hispanic | 236 (7.8) | 84.3 | 269 (9.6) | 75.0 | -9.3 |
| Educational | |||||
| Some college education or less | 921 (47.6) | 74.0 | 841 (41.4) | 74.4 | 0.4 |
| Associate or bachelor’s degree | 524 (30.4) | 88.8 | 504 (30.8) | 86.9 | -1.9 |
| More than college degree | 941 (21.9) | 85.8 | 1,056 (27.7) | 82.8 | -3 |
| Location of primary workplace|| | |||||
| Rural | 345 (14.7) | 74.2 | 283 (11.8) | 78.4 | 4.2 |
| Non-rural | 2,041 (85.3) | 82.3 | 2,118 (88.2) | 80.9 | -1.4 |
| Region¶ | |||||
| Northeast | 393 (19.4) | 78.3 | 455 (19.1) | 80.5 | 2.2 |
| Midwest | 291 (22.0) | 80.2 | 370 (22.0) | 80.6 | 0.4 |
| South | 1,291 (35.6) | 83.6 | 1,016 (36.4) | 80.5 | -3.1 |
| West | 411 (22.9) | 80.2 | 560 (22.6) | 80.8 | 0.6 |
| Occupation** | |||||
| Physician | 234 (3.2) | 96.7 | 236 (3.2) | 98.0 | 1.3 |
| Nurse practitioner/Physician assistant | 118 (1.2) | 91.0 | 136 (1.2) | 88.8 | -2.2 |
| Nurse | 193 (18.4) | 91.8 | 174 (18.1) | 92.0 | 0.2 |
| Pharmacist | 314 (1.3) | 91.5 | 307 (1.3) | 90.6 | -0.9 |
| Assistant/Aide | 588 (23.4) | 72.5 | 614 (23.5) | 72.4 | -0.1 |
| Other clinical personnel | 601 (20.9) | 85.8 | 589 (21.1) | 81.7 | -4.1 |
| Non-clinical personnel | 311 (31.3) | 75.5 | 316 (31.3) | 76.7 | 1.2 |
* Persons who worked in a place where clinical care or related services were provided to patients, or whose work involved face-to-face contact with patients or who were ever in the same room as patients.
† Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata (formerly Survey Sampling International).
‡ Weights were calculated based on each occupation type, by age, sex, race/ethnicity, work setting, and U.S. Census region to represent the U.S. population of HCP.
§ Race/ethnicity was self-reported. Persons identified as Hispanic might be of any race. The “other” race category included Asians, American Indians or Alaska Natives, Native Hawaiians or other Pacific Islanders, and persons who selected “other” or multiple races.
|| Rurality was defined using ZIP codes where more than 50% of its population resides in either a Non-Metro County and/or a rural Census Tract, according to the U.S. Health Resources & Services Administration’s definition of rural population (https://www.hrsa.gov/rural-health/about-us/definition/index.html).
¶ Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin. South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
** Other clinical personnel category includes allied health professionals, technicians, and technologists. Nonclinical personnel category includes administrative support staff members or managers and nonclinical support staff members (e.g., food service workers, laundry workers, janitors, and other housekeeping and maintenance staff members).
Table 2: Percentage of health care personnel* who received influenza vaccination by work-related characteristics, high-risk status, and employer vaccination policy, Internet panel surveys,† United States, April 2020
| Characteristics |
Total |
Employer vaccination requirement‡ |
No employer vaccination requirement |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Offered onsite vaccination >1 day§ |
Offered onsite vaccination 1 day|| |
Other vaccination promotion¶ |
No onsite vaccination or promotion |
|||||||||
|
No. (weighted %**) |
% (weighted) vaccinated |
No. (weighted %**) |
% (weighted) vaccinated |
No. (weighted %**) |
% (weighted) vaccinated |
No. (weighted %**) |
% (weighted) vaccinated |
No. (weighted %**) |
% (weighted) vaccinated |
No. (weighted %**) |
% (weighted) vaccinated |
|
| Total | 2,401 (100) | 80.6 | 960 (44.2) | 94.4 | 331 (11.7) | 89.4 | 304 (12.5) | 74.9 | 258 (11.9) | 73.3 | 548 (19.7) | 52.3 |
| Work Setting | ||||||||||||
| Hospital†† | 767 (100) | 93.2 | 560 (72.1) | 95.7 | 96 (12.4) | 92.5 | 73 (10.4) | 91.9 | (—‡‡) | —‡‡ | (—‡‡) | —‡‡ |
| Ambulatory care/ Physician office|||| | 693 (100) | 78.8§§ | 310 (42.9) | 96.1 | 104 (14.2) | 87.3§§ | 91 (12.3) | 80.2§§ | 41 (6.4) | 57.8 | 147 (24.1) | 47.7 |
| Long-term care | 569 (100) | 69.3§§ | 147 (29.0) | 88.9§§ | 47 (7.6) | 84.6§§ | 68 (14.0) | 60.6§§ | 97 (19.7) | 70.1 | 210 (29.7) | 49.0 |
| Other clinical setting¶¶ | 703 (100) | 77.7§§ | 183 (31.0) | 84.7§§ | 126 (10.3) | 89.2 | 104 (11.9) | 67.1§§ | 111 (21.7) | 89.1 | 179 (25.0) | 59.6 |
| High-risk conditions*** | ||||||||||||
| Yes †† | 736 (100) | 82.1 | 297 (46.0) | 91.2 | 92 (11.4) | 84.4 | 79 (10.5) | 75.9 | 95 (13.9) | 81.0 | 173 (18.2) | 61.9 |
| No | 1,665 (100) | 79.8 | 663 (43.2) | 96.2§§ | 239 (11.8) | 92.0§§ | 225 (13.5) | 74.5 | 163 (10.8) | 68.1§§ | 375 (20.6) | 47.9§§ |
| Occupation | ||||||||||||
| Clinical professional††, ††† | 1,164 (100) | 88.7 | 569 (56.9) | 97.9 | 197 (16.8) | 91.8 | 123 (7.3) | 89.2 | 76 (4.6) | 59.4 | 199 (14.5) | 58.5 |
| Clinical paraprofessional‡‡‡ | 921 (100) | 76.3§§ | 256 (30.3) | 97.4 | 103 (9.6) | 87.6 | 132 (15.5) | 70.3§§ | 147 (18.2) | 79.3§§ | 283 (26.5) | 49.6§§ |
| Non-clinical§§§ | 316 (100) | 76.7§§ | 135 (46.5) | 87.7§§ | 31 (8.6) | 86.9 | 49 (14.7) | 73.0§§ | 35 (12.5) | 68.9§§ | 66 (17.7) | 51.7§§ |
* Persons who worked in a place where clinical care or related services were provided to patients, or whose work involved face-to-face contact with patients or who were ever in the same room as patients.
† Respondents were recruited from two preexisting national opt-in Internet sources: Medscape, a medical website managed by WebMD Health Professional Network, and general population Internet panels operated by Dynata (formerly Survey Sampling International).
‡ Includes all respondents who indicated that their employer required them to be vaccinated for influenza.
§ Employer made influenza vaccination available on-site for >1 day during the influenza season at no cost to employees. Restricted to respondents without an employer requirement for vaccination.
|| Employer made influenza vaccination available on-site for 1 day during the influenza season at no cost to employees. Restricted to respondents without an employer requirement for vaccination.
¶ Influenza vaccination was promoted among employees through public identification of vaccinated persons, financial incentives or rewards to individuals or groups of employees, competition between units or care areas, free or subsidized cost of vaccination, personal reminders to be vaccinated, or publicizing of the number or percentage of employees receiving vaccination.
** Weights were calculated based on each occupation type, by age, sex, race/ethnicity, work setting, and U.S. Census region to represent the U.S. population of HCP.
†† Referent group for comparison within subgroups.
‡‡ Estimates with sample size <30 are not reported.
§§ ≥5 percentage-point difference compared with referent group.
|||| Ambulatory care (physician’s office, medical clinic, and other ambulatory care setting).
¶¶ Dentist office or dental clinic, pharmacy, laboratory, public health setting, health care education setting, emergency medical services setting, or other setting where clinical care or related services was provided to patients.
*** High risk conditions include diabetes, heart disease, lung disease, asthma, neurologic or neuromuscular problem, weakened immune system, kidney disease, blood disorders, and pregnancy.
††† Physicians, dentists, nurse practitioners, physician assistants, nurses, allied health professionals, pharmacists, and students in a medical-related field.
‡‡‡ Technicians/technologists; emergency technicians, paramedics, and EMTs; and assistants/aides.
§§§ Administrative support staff/managers, housekeeping and food service staff, and other nonclinical support staff.
Authors: Cristian Acero, MPH1,2; Hilda Razzaghi, PhD2; Carla L. Black, PhD2; Meredith G. Wesley, MPH3; Zuha Jeddy, MPH3; Megan C. Lindley, MPH2; Marie A. de Perio, MD4; A. Scott Laney, PhD5; Peng-Jun Lu, MD, PhD2; Walter W. Williams, MD2
1Kapili Government Services, LLC., Atlanta, GA; 2Immunization Services Division, National Center for Immunization and Respiratory Diseases, CDC; 3Abt Associates, Inc., Atlanta, GA; 4Office of the Director, National Institute for Occupational Safety and Health, CDC; 5Division of Respiratory Health, National Institute for Occupational Safety and Health, CDC.
Footnotes
*Physicians, nurse practitioners, physician assistants, nurses, dentists, pharmacists, allied health professionals, technicians, and technologists were recruited from the current membership roster of Medscape. Additional information on Medscape is available at https://www.medscape.com.
†Assistants, aides, and nonclinical personnel (such as administrators, clerical support workers, janitors, food service workers, and housekeepers) were recruited from general population Internet panels operated by Dynata. Additional information on Dynata and its incentives for online survey participants is available at https://www.surveysampling.com.
‡Population control totals of U.S. health care personnel by occupation and work setting were obtained from the Bureau of Labor Statistics, U.S. Department of Labor, Occupational Employment Statistics, May 2016 National Industry-Specific Occupational Employment and Wage Estimates (https://www.bls.gov/oes/current/oessrci.htm). Population control totals by other demographic characteristics were obtained from the U.S. Census Bureau, Current Population Survey Monthly Labor Force Data, September 2018 (https://www.bls.gov/cps/data.htm).
§Additional information on obstacles to inference in nonprobability samples is available at: https://www.aapor.org/AAPOR_Main/media/MainSiteFiles/NPS_TF_Report_Final_7_revised_FNL_6_22_13.pdf and https://www.aapor.org/getattachment/Education-Resources/For-Researchers/AAPOR_Guidance_Nonprob_Precision_042216.pdf.aspx. While the estimates reported here have variance, there has been no attempt to quantify the size of the variance.
||A survey response rate requires specification of the denominator at each stage of sampling. During recruitment of an online opt-in survey sample, such as the Internet panels described in this report, these numbers are not available; therefore, a response rate cannot be calculated. Instead, the survey completion rate is provided.
- Centers for Disease Control and Prevention (CDC). Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2011;60(RR-7):1-45.
- Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333(7581):1241-1244.
- Lemaitre M, Meret T, Rothan-Tondeur M, et al. Effect of influenza vaccination of nursing home staff on mortality of residents: a cluster-randomized trial. J Am Geriatr Soc. 2009;57(9):1580-1586.
- Saxen H, Virtanen M. Randomized, placebo-controlled double-blind study on the efficacy of influenza immunization on absenteeism of health care workers. Pediatr Infect Dis J. 1999;18(9):779-783.
- Worksite: Seasonal influenza vaccinations using interventions with on-site, free, actively promoted vaccinations – healthcare workers. Community Preventive Services Task Force website. https://www.thecommunityguide.org/findings/worksite-seasonal-influenza-vaccinations-healthcare-on-site. Accessed June 16, 2020.
- Bardenheier B, Lindley MC, Yue X, et al. Influenza vaccination coverage among health care personnel — United States, 2018–19 influenza season. Atlanta, GA: US Department of Health and Human Services, CDC; 2019. https://www.cdc.gov/flu/fluvaxview/hcp-coverage_1819estimates.htm
- Black CL, Yue X, Ball SW, et al. Influenza vaccination coverage among health care personnel — United States, 2017–18 influenza season. MMWR Morb Mortal Wkly Rep 2018;67:1050–1054.
- Closing the gap in a generation: Health equity through action on the social determinants of health. Geneva: World Health Organization; 2008. Available at: http://whqlibdoc.who.int/hq/2008/WHO_IER_CSDH_08.1_eng.pdf.Accessed June 16, 2020.
- McMichael TM, Clark S, Pogosjans S, et al. COVID-19 in a long-term care facility — King county, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep 2020;69:339-342.
- Lu PJ, Hung MC, O’Halloran AC, et al. Seasonal influenza vaccination coverage trends among adult populations, U.S., 2010-2016. Am J Prev Med. 2019;57(4):458-469.