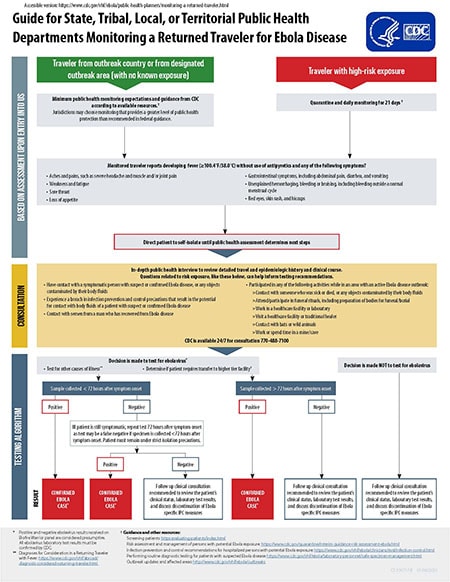
Guide for State, Tribal, Local, or Territorial Public Health Departments Monitoring a Returned Traveler for Ebola Disease
Print this guide [PDF – 1 page] for help with monitoring a returned traveler for Ebola disease.
After entry into the United States
Travelers from an outbreak country or from a designated outbreak area (with no known exposure) will experience minimum public health monitoring expectations and guidance from CDC based on available resources.
Travelers who have reported a high-risk exposure should quarantine and be monitored daily for 21 days.
Any monitored traveler reporting fever (100.4°F/38.0°C) without use of antipyretics and any of the following symptoms should be directed to self-isolate until public health assessment determines next steps.
- Aches and pains, such as severe headache and muscle and/or joint pain
- Weakness and fatigue
- Sore throat
- Loss of appetite
- Gastrointestinal symptoms, including abdominal pain, diarrhea, and vomiting
- Unexplained hemorrhaging, bleeding or bruising, including bleeding outside a normal menstrual cycle
- Red eyes, skin rash, and hiccups
Consultation with clinical team for testing recommendations of patients with an exposure risk and symptoms compatible with Ebola disease
An in-depth public health interview will be conducted with the clinical team to review a detailed travel and epidemiologic history and clinical course of the patient. Questions related to risk exposure, like these below, can help inform testing recommendations.
Did the patient:
- Have contact with a symptomatic person with suspected or confirmed Ebola disease, or any objects contaminated by their body fluids?
- Experience a breach in Infection Prevention and Control (IPC) precautions that result in the potential for contact with body fluids of a patient with suspected or confirmed Ebola disease?
- Have contact with semen from a man who has recovered from Ebola disease?
- Participate in any of the following activities while in an area with an active Ebola disease outbreak?
- Contact with someone who was sick or died, or any objects contaminated by their body fluids
- Attend/participate in funeral rituals, including preparation of bodies for funeral/burial
- Work in a healthcare facility or laboratory
- Visit a healthcare facility or traditional healer
- Contact with bats or wild animals
- Work or spend time in a mine/cave
As a resource for State, Tribal, Local, or Territorial public health departments, CDC is available 24/7 for consultation 770-488-7100.
Testing algorithm
Through the consultation process, if the decision is made to test for ebolavirus, testing for other causes of illness should continue (refer to Performing routine diagnostic testing for patients with suspected Ebola disease for guidance). In addition, a determination should be made on whether the patient requires transfer to a higher tier facility. If the decision is made NOT to test for ebolavirus, a follow up clinical consultation is recommended to review the patient’s clinical status and laboratory test results and to discuss discontinuation of Ebola specific IPC measures.
When the decision has been made to test the patient, the following testing algorithm can be used:
If a sample is collected less than 72 hours after symptom onset and tests positive, the patient is considered a confirmed Ebola case*. If the sample tests negative and the patient is still symptomatic, the test should be repeated 72 hours after symptom onset as the test may produce a false negative if the specimen is collected less than 72 hours after symptom onset. The patient must remain under strict isolation precautions during this time.
If the test is repeated 72 hours after symptom onset and the test is positive, the patient is considered a confirmed Ebola case*. If the test is negative, a follow up clinical consultation is recommended to review the patient’s clinical status and laboratory test results and to discuss discontinuation of Ebola specific IPC measures.
If the initial sample is collected over 72 hours after symptom onset and the test is positive, the patient is considered a confirmed Ebola case*. If the test is negative, a follow up clinical consultation is recommended to review the patient’s clinical status and laboratory test results and to discuss discontinuation of Ebola specific IPC measures.
* Positive and negative ebolavirus results received on a Biofire Warrior panel are considered presumptive. All ebolavirus laboratory test results must be confirmed by CDC.
Reporting Confirmed Cases of Ebola Disease to CDC
Learn more on case reporting recommendations at Domestic Ebola Disease Case Reporting Recommendations for Health Departments.